21 Comments
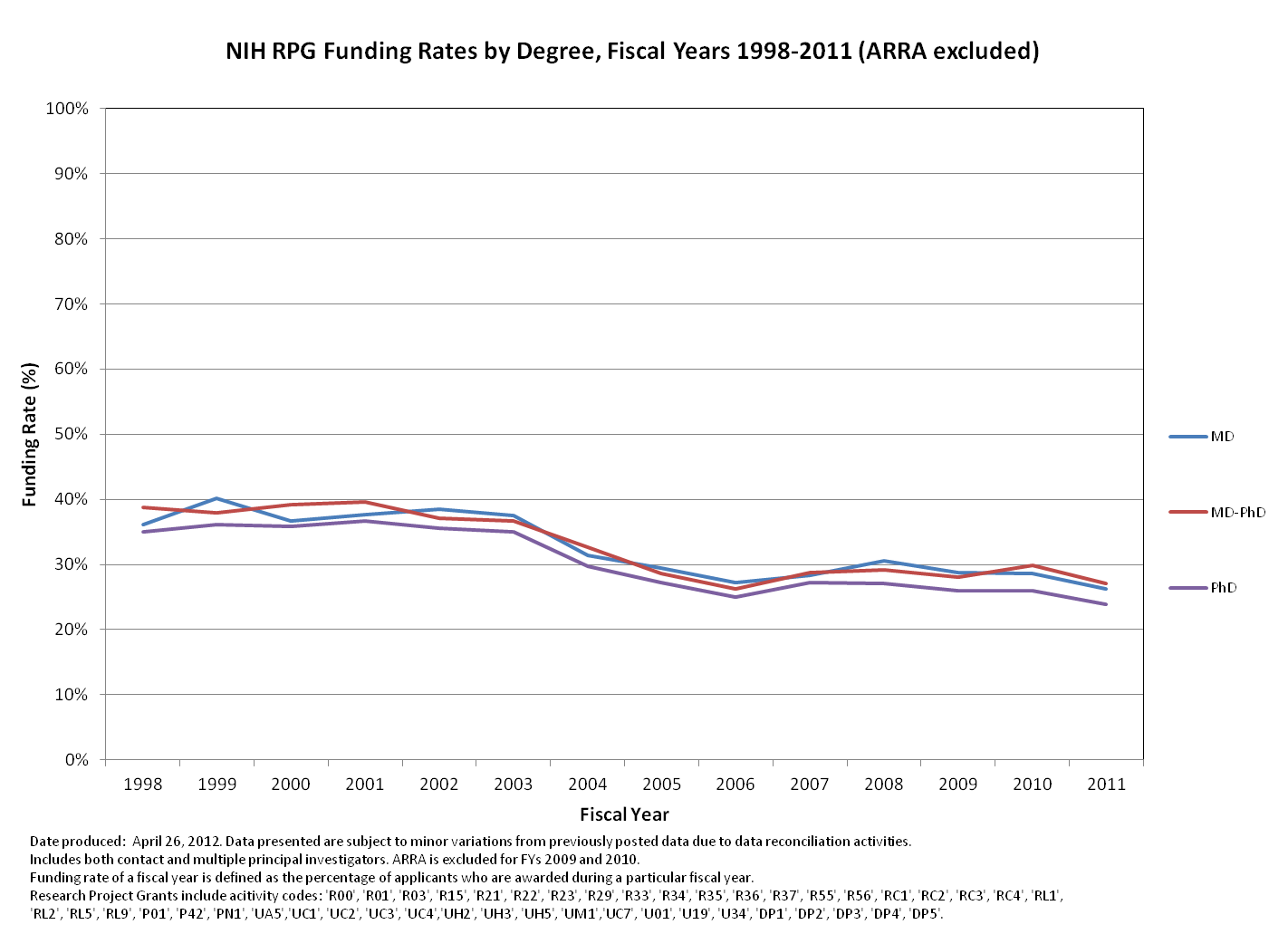
If you are a regular reader of my blog, you know I like to try and provide data that answer commonly asked questions about NIH funding. Today, it’s the question of whether investigators that hold MDs or MD/PhDs are more or less likely to be funded than those investigators that hold PhDs. Well, in this case, there is a difference, but it is modest.
Investigators with a PhD have a slightly lower funding rate than those with medical degrees, and this is consistent over time. Note that this is the funding rate, which is the percentage of applicants that receive funding in a fiscal year. By comparison, our success rate is calculated on the project level, not the person, and as you all know is much lower. To keep these data in context, remember that about 30% of principal investigators hold MDs or MD/PhDs.
We know that the types of degrees that investigators hold vary based on the type of institution at which that they work, so next we will look to see if there are any differences in the funding rate by degree when broken down by institution type.
Interested in the raw numbers? Check out NIH Research Project Grants: Funding rates by degree, FY98-11 on RePORT.



OK, so this is saying that 30% of PIs calculated in the ‘funding rate’ hold a Md or Md/Phd, but this pool represents ~60% of the ‘funding rate'(combining the Md/Phd and MD pools?)? How in the world is that a modest difference? And why is a ‘funding rate’ metric possibly useful?
NIH tends to comb through data to feign equality..
What about making taxpayer funded study section review scores public for funded grants? I would suspect MDs may receive much worse scores, but much more preference when it comes to funding decisions… but we’ll never know, will we?
To clarify, the funding rate reflects the percentage of people that are funded in a particular year. This is different from our success rate, which shows the percentage of projects that are funded in a particular year. So what this graph shows is the rate at which investigators that hold these various degrees get funded. The absolute numbers of MD or MD/PhD investigators that get funded are much less than PhD investigators, roughly 30/70.
The funding rate is incredibly valuable! It let’s us know if the pool of investigators seeking/winning funding is changing independently from changes in grant submitting behavior. Different concerns and solutions involved with increasing apps from the same number of investigators versus increasing numbers of investigators seeking funding. Similar deal when trying to determine if a given policy is having any effect.
The real problem is that the US PhD-trained academic researcher recently found himself/herself in a socialized global science profession (do-gooders with an unprotected labor supply vs. demand) whereas the US MD is currently in a national health care profession (very protected in numbers and lucrative). Simple economics. The universities, medical profession, CEOs etc. lobbied for this (a US congressman told me this) and have used this to their advantage by means we all know too well. Of course, it hasn’t necessarily equated to the best health care or science for the US. Eliminating the ‘mega’ grants is one easy remedy for rebalancing PhD supply-demand, improving the quality and integrity of medical research, the recruitment and retainment of top US scientists, and fairness in grant competition. Someone should do the numbers, but not in an Orwellian manner. For example, how many H1B post-docs did the NIH and US govt. support during the 1995-2004 bubble vs. before or after (did it coincide with the unsustainable >1 trillion dollar foreign debt)? How many of those H1B scientists remain in the funding system as post-docs or non-tenured faculty at medical centers?
I’m not keen on the rather poorly hidden racist undertones in your message. The time limit on the H1B visa is 6 years, so very few H1Bs remain from the mid-2000s as post-doc’s or non-tenured faculty today. After 6 years it’s apply for permanent residency or go home. Only those with good publication records and have made a strong contribution to the field can get a green card (I know because I’m one of them, and for the record I currently employ 3 US citizens in my lab). There is simply no evidence for a mass of former H1B post-doc’s clogging the system and stopping US citizens from getting jobs. But of course, blaming the current job market on immigrants is always an easy option.
As for the “globalized” science market, anyone who sees this as a problem is somewhat blind to the overt snobbery of US born post-doc’s. Unless you happen to be in the northeast corridor or the west coast, young US post-doc’s are simply not interested in moving to your small city. The world is their oyster, and they’re gonna go where the social life is good and/or the sun shines a lot. Why would an unmarried 26 year old want to move to rust-belt Ohio or suburban sprawl-ville Texas? I ran an ad’ last year in a prominent magazine and online, and received over 120 applications from India and China, and exactly zero from the US. Nada. Zilch. This despite my lab averaging 12 publications last year in top-rank journals, and a strong track record of graduates going on to get good positions. If I could get US post-doc’s to apply, I would hire them in a snap (and have in the past) but the smart kids all wanna be in NYC or SF these days, not in the snow-belt. Foreign born scientists are less picky about this.
You know we have the same problem with health care in the US. The best MDs tend to gravitate to the nice areas, and health care is rather poor in many rural and urban areas. The costs are also high even in the nice places. Perhaps increased immigration in medicine would also be the answer. I wonder why we have not done that more? Come to think of it, there are many professions that may benefit from the strategy you support.
The fact that the US PhD-trained researchers are in a global profession cannot be construed as being bad. If anything, the US trained researcher had access to the best mentorship, equipment, opportunities. He/she would better be able to compete with the outside of US trained researcher. If he/she loses, I guess that’s what happens with those who cannot make the cut. The fact that MDs are in a health care profession is explained by the choice they made to go medical school. I find it hard to believe that you were mislead when starting your PhD and thought all along that you will be in the health care profession upon graduation. I believe I don’t need to give other examples, but the best case scenario is graduation with a degree that you applied for and was accepted for. As to what happens in clinical medicine, this is as relevant to this discussion as what happens with Walmart employees. Equally irrelevant is what a “senator” related to you, in which context, how you understood it, and how you relate that fact. Finally, the suggestion that the US debt is due (at least in significant proportion) to the large numbers of foreign scientists on H1B visas, is downright ludicrous. Along the lines of same conspiracy, do you really think that a PI would even consider dealing with the headaches of hiring somebody from a foreign country, sight unseen, less rigorously trained that a US PhD graduate, and having to deal with visa issues, etc, if there were choices?? Really? Is everybody (foreign trained scientists, US doctors, senators, lobbyists, medical professionals and CEOs (?!) ) conspiring against your successful application for an RO1?
I think not. Be competitive and, as the NIH statistics demonstrate, your chances are same, regardless of your titles (MD vs. PhD vs. MD/PhD).
I was on an NIH training fellowship during a good part of my doctoral training with a pay-back agreement specifying that I would serve the US Public Health Service for 2-3 years doing health-related research. I dutifully did that of course. What bothers me is the purposefully, or mistakenly, putting too many mice in the cage. Nothing wrong with putting mice in cages mind you, just too many is the problem. I suppose you will think that is also irrelevant. Who is putting the mice in the cages to ‘make the cut’ you speak of. Is everyone doing it? When I say mice, I mean the junior investigators (anyone) who you suggest really have been promised nothing for a career in health care. I think you are the one mistaken about what the young investigators expect and deserve for successfully completing that step of their training. Sad 🙁
Note the words “health care” above were often used instead of the more exact description health care research, or biomedical research. However, the meanings should have been for the most part clear when referring to what the MD profession and PhD professions are traditionally trained for by their specific graduate degree programs. MD = health care (clinical) and PhD = health care (biomedical research). Sorry for the confusion this simple omission causes. My point nevertheless remains that labor supply has not been sufficiently restrained in the biomedical research profession and has caused problems for the profession and especially at the PhD training stages that you refer to as enviable in the US. I see that the NIH workforce study group had also said something similar, but it was not widely publicized!!
No, Title matters for average minds. Unless you are already on top or in a top lab.
How about a parallel assessment of PhD vs. RN/PhD? There are a number of RN investigators who believe the RN hampers funding.
I’m impressed (and more than a little dismayed) at the strong “sour grapes” tone to many of the posts by PhD reseachers so far. Rather than invoking conspiracy theories, preferential treatment by reviewers and funding officials, and the like, I simply suspect MD-led proposals may be most likely to address pressing clinically and health policy relevant issues.
Also as Rock Talk Blog Team points out, the absolute number of MDs funded is much less than the number of PhDs, so a lot of the bluster in the prior posts simply reflects a poor understanding of the data being presented.
MD writes better for pressing clinically and health-relevant issues, they should be supported for their research.
Those people work with passion, and less stress in terms of salary compared to PhDs.
Basic science got less care, that’s where the sour grapes came from.
I sense an anti-MD bias from our PhD colleague. His conclusion that 30% of the applicant pool (MD, MD/PhD) obtain 60% of funds is grossly inaccurate. My take on this graph is that a candidate from ANY of theses three pools (PhD, MD, MD/PhD) has ~30% chance of funding. The NIH awards have likely been made in these same percentages.
How about this question? What is the NIH funding rate for MDs or MD/PhDs with more than two months of clinical service? Or, do you think clinical insight into a biomedical problem actually counts for anything? I can’t tell you how many times I have heard some bonehead extrapolation of a cell culture finding to finding “a cure” for human disease, including from a host of want-to-be Lasker or Nobel Awardees. Better yet, if they are more “translationally” oriented, they want to brag how they cure disease in a mouse model. The bias against proposals that use patient-derived cell lines or samples or, worse yet, pilot human clinical studies that “skip” a mouse model is incredibly blatant for those who open their eyes. Not that mouse studies cannot be helpful, but even here most PhDs are like a fish out of water. Medical school and residency/fellowship actually teach you a thing or two about mammalian physiology or pathophysiology, which is rather easily applied to the mouse or rat. By the way, a graduate student cannot learn this information in some bogus semester graduate class, like some schools at trying to do now (at the behest of the NIH). Do you really think the medical students are so dumb that it takes them years and years to learn this material???
As far as absolute numbers, the NIH and its review panels have been dominated by PhD investigators (~75%) including many who have promised to deliver cures, yet have fallen short time and time again. No wonder the public is tiring of the snake oil sales pitch from the NIH and their PhD cronies. Maybe the wars on AIDS, cancer, and heart disease have not been won because it is like asking an electrician to come in and fix a leak, in this case a torrent of water. I say let’s split the NIH funds 50:50 and let the PhDs, non-clinician MDs, non-clinician MD/PhDs go at at against clinician-investigators on human disease projects. By the way, curing human disease in worms and flies won’t count.
I have had MD’s and PhD’s in my labs and and while there maybe exceptions in the MD’s by far most of them have to be retrained to think critically and with more then a memorized textbook view. (which is pretty much how most they are trained in medical school). I would even venture to ask PS13 to name a few MD’s who actually conceived /designed (or came up) with any modern drug that is used for treatment. Oh yes… after the computational or medicinal chemists and the other scientist who do all the optimizing in animals etc for PK/PD and efficacy are done with the development. Then all the MD’s (because they have control of patient recruitment and patient access) get the drug handed to them to see and prove that it does work (as conceived/ designed and provided by the PhD scientist). Most of the credit and glory ends up going to the MD’s as “they have successfully tested a drug that works and here is the clinical trial !!
So my question to PS 13 is …who is the innovator here… the PhD scientist that conceived, designed and make the drugs that we use today in modern medicine ….. or the MD who tested it in the patient (most MD’s and disease specialist are apriori told what drug is for and how to test it)…??
I am a bit puzzled at this rather sterile debate. What we are all in for, regardless of our initial training, is delivering safe and efficacious treatment to patients with unmet medical needs. My modest view on this debate is that bringing these complex drugs to the patient bedside requires contribution from many folks, from preclinical and early clinical science, medicine, but also patient care (research nurses in particular), business, regulatory (very often PharmD), none being less essential than another, whether they come from public or for-profit institutions. Ultimately, we should be lucky that patients even agree to trust us with their health when they participate to cliincal trials. In other words, it’s all about TEAM WORK, and folks arguing whether their “label” (obtained in their 20s) is better than their neighbors aren’t probably focusing enough on what’s ultimately good for patients and society in general.
OK, yes I will agree I did not interpret the ‘funding rate’ metric correctly.
I still don’t really understand the point though. Are these data including only people who, at one time or another, were PIs? Or including people who have never been a PI? You’d need to separate that out to interpret.
However, I still contend there are so many NIH-hidden metrics that would be more helpful as to what the chances the average person, MD or otherwise, has for funding themselves. The reason why the funding rate metric is not useful is that the awards are lumped together as if they are equal, as in if somebody is PI of an R03, that is counted the same as PI of a U01. What I am getting at is that I believe it is easier for an NIH funded MD (NOT the average MD, obviously) to support themselves from grant money than a NIH funded PhD. This is because the paylines are higher for the larger grants that more fully support salary.
But you really can’t tell what is happening from available NIH data. Hidden institute paylines (most of them), hidden section scores, hidden reviews, hidden agenda… Earmarked programs, particular PI-centric RFAs, etc.
You can make a case that the DOD and Pentagon need to be secretive for national security, but the NIH?
To Realities in Drug Discovery: Sure, the stereotypical medical student/resident/fellow is a master of facts, but do you really think they don’t perform deductive reasoning in their medical applications? A talented clinician uses the same logic as a talented basic scientist to arrive at a carefully conceived and executed research project. I would gladly have either of these individuals in my lab. The main problem with medically trained researchers is they are used to getting rapid feedback and many readily admit they don’t have the stomach for a prolonged haul required in solving a tough problem. However, many basic scientists I know have tunnel vision, but cloak it with pride by saying that they are taking “a reductionist approach” to their science. In reality, they are afraid or poorly trained to take on an entirely new problem.
And how about this? After years of heaving the most scathing comment on a grant or manuscript review as being “descriptive science”, the snake oil basic scientist salesman put on a new spin, “-omics or discovery science”, and now say this approach will open new avenues of research. Not that descriptive science is bad (is this heresy?!!!). After all, if we had an army of clinicians who just used reductionist approach based upon one piece of data without first processing the “descriptive data” to form a list of differential diagnoses (probably know better to you as hypotheses), there would be a lot of dead patients out there. Don’t think you own the rights to deductive logic. That’s why science in the US is in trouble, because the haughty basic scientists who “know better” are telling us (the public and the clinically-trained researcher) how and what to do without admitting that an alternative view or approach (by others – if it was them, it would be a spectacular idea) should be thoughtfully considered.
However, probably the bigger problem with modern science funded by the NIH (and practice by many researchers, all inclusive) is that it rewards those who superficially study an area and then move on to “the next important question”. Despite the sacred hypothesis testing, which is supposed to mark modern science, their is a lot of inaccurate, and often wrong, conclusions out there based upon poorly designed, executed, or interpreted studies – hence the 50% accuracy of Science/Nature/Cell reports. Perhaps if the NIH had a policy that one aim of a three aim R01 is okay if it mainly substantiates an earlier important claim, rather than penalize the PI for not being “innovative”, we would not have cases like the 80-90% lack of reproducibility as pointed out by the former head of cancer research at Amgen.
As far as MD contributors and medical advances, have you looked at the list of Nobel laureates in Medicine and Physiology? I would venture that there are a lot more MDs in that list compared to PhDs (not to say that there were not any fabulous contributions by PhDs) and certainly more of a percentage then that funded by the NIH. Not that MDs own the rights to insightful investigations and approaches. My most important role model is an old-time basic scientist who trained with a bigwig basic scientist and always reminds me that an in vitro experiment should be optimized to reflect what occurs in vivo rather than optimize it for in vitro kinetics. He also laments the dumbing down of the current bag of basic scientists, especially in his area, and notes with disdain that the snakeoil salesmen in his field (mostly, if not all, PhDs, by the way) periodically coin a new phrase or term for something that was discovered decades ago, but who now use their “novel finding” to secure a spotlight or piggier share of the limited funding pie. By the way, through the years, my role model had a lot of very talented MDs who performed most of his seminal findings.
What I and many of my colleagues who have MD/PhDs often felt was that it was questionable whether the +PhD component added enough in fund ability to justify 4+ extra years on top of 7+ years of medical training. Many times I was told that MDs could readily be funded for clinical investigation, and competing as a part-clinical faculty against full-time PhDs was having one hand tied behind your back. The attached graphic suggests a marginal advantage consistently over PhDs, but no real advantage systematically over MDs.
I would be interested in the percentage of DVM or DVM/PhD’s that are funded by NIH
The question is why have a PhD program at all? If the funding is the same if you have an MD or a PhD what is the advantage/reason for having a PhD? If a training in research does not equip a person to apply that training to do research any better than someone who has not been trained in research then I do not see a point in having a PhD program. It would seem to me that it is a huge waste of money, given that the success rate of a PhD is “slightly less” than that of an MD and a MD can always practice medicine to support themselves if they do not obtain funding from the NIH and a PhD does not have that option. A PhD would most likely apply the skills they have acquired toward a career in industry if they fail to obtain NIH funding and therefore tax payers would have spent a lot of money to train someone, whereas the majority of MD’s pay for their own training. Given the other comments I feel I am preaching to the choir here but I thought it was worth posing the question.